2024
Witt, Karsten; Levin, Johannes; van Eimeren, Thilo; Hasan, Alkomiet; Ebersbach, Georg; and Mathias Bähr,; Becktepe, Jos; Berg, Daniela; Brockmann, Kathrin; Buhmann, Carsten; Ceballos-Baumann, Andrés; Claßen, Joseph; Deuschl, Cornelius; Deuschl, Günther; Dodel, Richard; Ebersbach, Georg; Eggers, Carsten; van Eimeren, Thilo; Fanciulli, Alessandra; Fimm, Bruno; Folkerts, Ann-Kristin; Gausepohl, Madeleine; Hasan, Alkomiet; Hermann, Wiebke; Hilker-Roggendorf, Rüdiger; Höglinger, Günter; Höllerhage, Matthias; Hopfner, Franziska; Jost, Wolfgang; Kalbe, Elke; Kassubek, Jan; Klebe, Stephan; Klein, Christine; Klietz, Martin; Köglsperger, Thomas; Kühn, Andrea; Krack, Paul; Krismer, Florian; Kuhlenbäumer, Gregor; Levin, Johannes; Liepelt-Scarfone, Inga; Lingor, Paul; Loewenbrück, Kai; Löhle, Matthias; Lorenzl, Stefan; Maaß, Sylvia; Maetzler, Walter; Menzel, Regina; Meyer, Philipp T.; Mollenhauer, Brit; Neumann, Manuela; Odin, Per; Outeiro, Tiago; Pötter-Nerger, Monika; Reese, René; Reetz, Kathrin; Rieß, Olaf; Ruf, Viktoria; Schneider, Anja; Schrader, Christoph; Schnitzler, Alfons; Seppi, Klaus; Sixel-Döring, Friederike; Storch, Alexander; Tönges, Lars; Trenkwalder, Claudia; van Eimeren, Thilo; Walter, Uwe; Wächter, Tobias; Warnecke, Tobias; Wegner, Florian; Winkler, Christian; Witt, Karsten; Woitalla, Dirk; Zeuner, Kirsten; Bantel, Martina; Witt, Jonas L.
In: J Neurol, vol. 271, no. 12, pp. 7402–7421, 2024, ISSN: 1432-1459.
Abstract | Links | BibTeX | Tags: Guidelines, Impulse control disorder, Parkinson
@article{Witt2024,
title = {Diagnostics and treatment of impulse control disorders, psychosis and delirium: systemic review-based recommendations - guideline “Parkinson’s disease” of the German Society of Neurology},
author = {Karsten Witt and Johannes Levin and Thilo van Eimeren and Alkomiet Hasan and Georg Ebersbach and and Mathias Bähr and Jos Becktepe and Daniela Berg and Kathrin Brockmann and Carsten Buhmann and Andrés Ceballos-Baumann and Joseph Claßen and Cornelius Deuschl and Günther Deuschl and Richard Dodel and Georg Ebersbach and Carsten Eggers and Thilo van Eimeren and Alessandra Fanciulli and Bruno Fimm and Ann-Kristin Folkerts and Madeleine Gausepohl and Alkomiet Hasan and Wiebke Hermann and Rüdiger Hilker-Roggendorf and Günter Höglinger and Matthias Höllerhage and Franziska Hopfner and Wolfgang Jost and Elke Kalbe and Jan Kassubek and Stephan Klebe and Christine Klein and Martin Klietz and Thomas Köglsperger and Andrea Kühn and Paul Krack and Florian Krismer and Gregor Kuhlenbäumer and Johannes Levin and Inga Liepelt-Scarfone and Paul Lingor and Kai Loewenbrück and Matthias Löhle and Stefan Lorenzl and Sylvia Maaß and Walter Maetzler and Regina Menzel and Philipp T. Meyer and Brit Mollenhauer and Manuela Neumann and Per Odin and Tiago Outeiro and Monika Pötter-Nerger and René Reese and Kathrin Reetz and Olaf Rieß and Viktoria Ruf and Anja Schneider and Christoph Schrader and Alfons Schnitzler and Klaus Seppi and Friederike Sixel-Döring and Alexander Storch and Lars Tönges and Claudia Trenkwalder and Thilo van Eimeren and Uwe Walter and Tobias Wächter and Tobias Warnecke and Florian Wegner and Christian Winkler and Karsten Witt and Dirk Woitalla and Kirsten Zeuner and Martina Bantel and Jonas L. Witt},
doi = {10.1007/s00415-024-12576-x},
issn = {1432-1459},
year = {2024},
date = {2024-12-00},
urldate = {2024-12-00},
journal = {J Neurol},
volume = {271},
number = {12},
pages = {7402--7421},
publisher = {Springer Science and Business Media LLC},
abstract = {<jats:title>Abstract</jats:title><jats:sec>
<jats:title>Background and objective</jats:title>
<jats:p>Impulse control disorders (ICD), psychosis and delirium are part of the spectrum of behavioural changes associated with Parkinson’s disease (PD). The diagnostic and therapeutic management of these rather complex neuropsychiatric conditions has been updated in the clinical guideline by the German Society of Neurology (DGN).</jats:p>
</jats:sec><jats:sec>
<jats:title>Methods</jats:title>
<jats:p>Recommendations are based on a systematic literature reviews, other relevant guidelines and expert opinion.</jats:p>
</jats:sec><jats:sec>
<jats:title>Results</jats:title>
<jats:p>Patients receiving dopamine agonists (DA) therapy should be informed about the symptoms and risks of an ICD and should be routinely screened for ICD symptoms. In the presence of an ICD, DA should be reduced or discontinued and psychotherapeutic treatment may be considered. Non-oral therapies (levodopa/carbidopa intestinal gel infusion or deep brain stimulation) may also be an option for appropriate candidates. Psychosis in PD often has a gradual onset. Cognitive and affective disorders, psychiatric and medical comorbidities as well as polypharmacy are risk factors for a psychosis. Non-pharmacological treatments should be implemented as soon as possible and anti-parkinsonian medications should be adjusted/reduced if feasible. For psychosis associated with PD, quetiapine or clozapine should be used on an as-needed basis and for as short a time as is necessary, with safety monitoring. Delirium in PD may be underdiagnosed due to an overlap with chronic neuropsychiatric features of PD. Although transient by definition, delirium in PD can lead to permanent cognitive decline, motor impairment and increased mortality. Management of delirium includes pharmacological and non-pharmacological interventions.</jats:p>
</jats:sec><jats:sec>
<jats:title>Conclusion</jats:title>
<jats:p>The updated guideline encompasses the evidence-based diagnostic, non-pharmacological and pharmacological management of ICD, psychosis and delirium in PD.</jats:p>
</jats:sec>},
keywords = {Guidelines, Impulse control disorder, Parkinson},
pubstate = {published},
tppubtype = {article}
}
<jats:title>Background and objective</jats:title>
<jats:p>Impulse control disorders (ICD), psychosis and delirium are part of the spectrum of behavioural changes associated with Parkinson’s disease (PD). The diagnostic and therapeutic management of these rather complex neuropsychiatric conditions has been updated in the clinical guideline by the German Society of Neurology (DGN).</jats:p>
</jats:sec><jats:sec>
<jats:title>Methods</jats:title>
<jats:p>Recommendations are based on a systematic literature reviews, other relevant guidelines and expert opinion.</jats:p>
</jats:sec><jats:sec>
<jats:title>Results</jats:title>
<jats:p>Patients receiving dopamine agonists (DA) therapy should be informed about the symptoms and risks of an ICD and should be routinely screened for ICD symptoms. In the presence of an ICD, DA should be reduced or discontinued and psychotherapeutic treatment may be considered. Non-oral therapies (levodopa/carbidopa intestinal gel infusion or deep brain stimulation) may also be an option for appropriate candidates. Psychosis in PD often has a gradual onset. Cognitive and affective disorders, psychiatric and medical comorbidities as well as polypharmacy are risk factors for a psychosis. Non-pharmacological treatments should be implemented as soon as possible and anti-parkinsonian medications should be adjusted/reduced if feasible. For psychosis associated with PD, quetiapine or clozapine should be used on an as-needed basis and for as short a time as is necessary, with safety monitoring. Delirium in PD may be underdiagnosed due to an overlap with chronic neuropsychiatric features of PD. Although transient by definition, delirium in PD can lead to permanent cognitive decline, motor impairment and increased mortality. Management of delirium includes pharmacological and non-pharmacological interventions.</jats:p>
</jats:sec><jats:sec>
<jats:title>Conclusion</jats:title>
<jats:p>The updated guideline encompasses the evidence-based diagnostic, non-pharmacological and pharmacological management of ICD, psychosis and delirium in PD.</jats:p>
</jats:sec>
Dzialas, Verena; Doering, Elena; Eich, Helena; Strafella, Antonio P.; Vaillancourt, David E.; Simonyan, Kristina; van Eimeren, Thilo
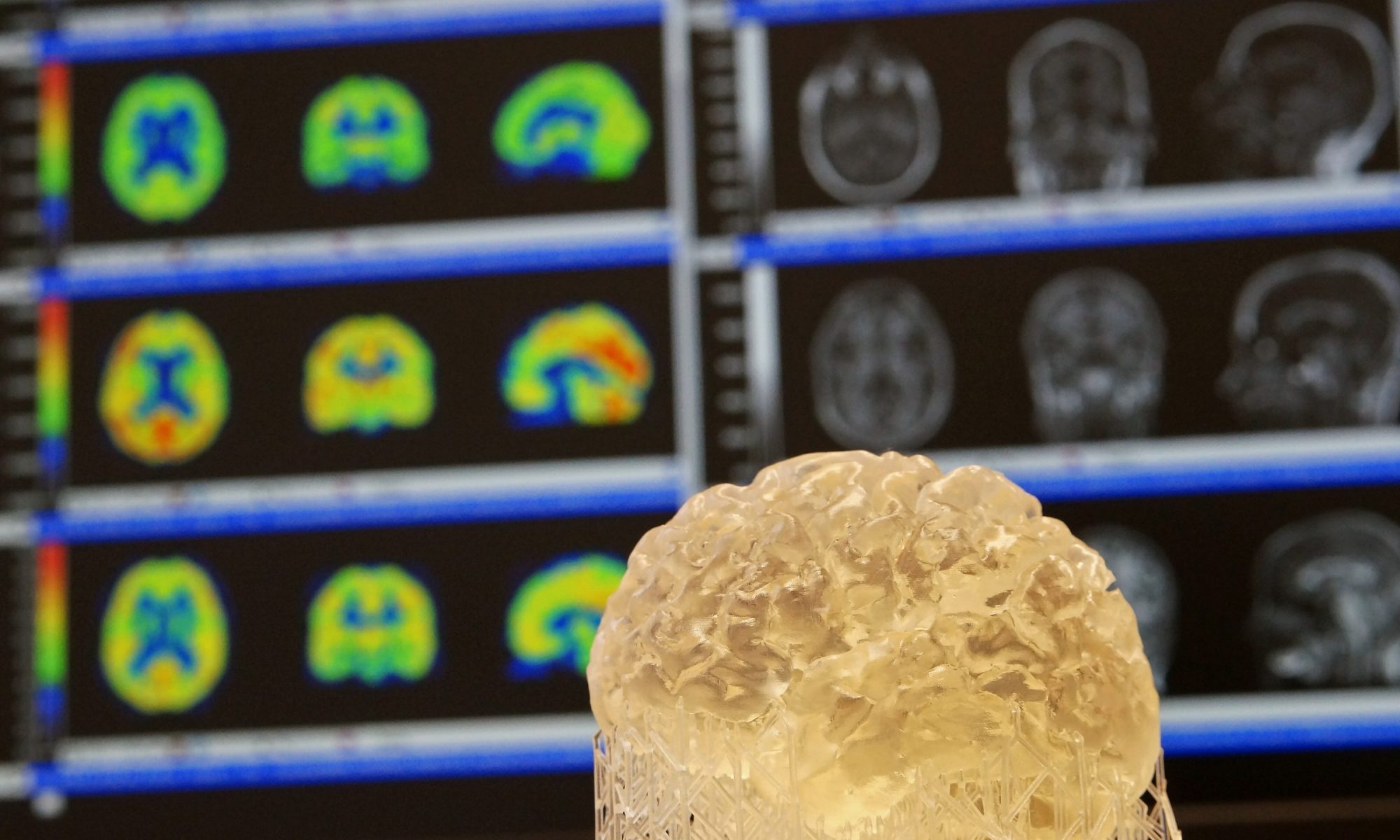
Houston, We Have AI Problem! Quality Issues with Neuroimaging‐Based Artificial Intelligence in Parkinson's Disease: A Systematic Review Journal Article
In: Movement Disorders, vol. 39, no. 12, pp. 2130–2143, 2024, ISSN: 1531-8257.
Abstract | Links | BibTeX | Tags: Artificial Intelligence, DaT imaging, Guidelines, Parkinson, Structural MRI
@article{Dzialas2024,
title = {Houston, We Have AI Problem! Quality Issues with Neuroimaging‐Based Artificial Intelligence in Parkinson's Disease: A Systematic Review},
author = {Verena Dzialas and Elena Doering and Helena Eich and Antonio P. Strafella and David E. Vaillancourt and Kristina Simonyan and Thilo van Eimeren},
doi = {10.1002/mds.30002},
issn = {1531-8257},
year = {2024},
date = {2024-12-00},
urldate = {2024-12-00},
journal = {Movement Disorders},
volume = {39},
number = {12},
pages = {2130--2143},
publisher = {Wiley},
abstract = {In recent years, many neuroimaging studies have applied artificial intelligence (AI) to facilitate existing challenges in Parkinson's disease (PD) diagnosis, prognosis, and intervention. The aim of this systematic review was to provide an overview of neuroimaging‐based AI studies and to assess their methodological quality. A PubMed search yielded 810 studies, of which 244 that investigated the utility of neuroimaging‐based AI for PD diagnosis, prognosis, or intervention were included. We systematically categorized studies by outcomes and rated them with respect to five minimal quality criteria (MQC) pertaining to data splitting, data leakage, model complexity, performance reporting, and indication of biological plausibility. We found that the majority of studies aimed to distinguish PD patients from healthy controls (54%) or atypical parkinsonian syndromes (25%), whereas prognostic or interventional studies were sparse. Only 20% of evaluated studies passed all five MQC, with data leakage, non‐minimal model complexity, and reporting of biological plausibility as the primary factors for quality loss. Data leakage was associated with a significant inflation of accuracies. Very few studies employed external test sets (8%), where accuracy was significantly lower, and 19% of studies did not account for data imbalance. Adherence to MQC was low across all observed years and journal impact factors. This review outlines that AI has been applied to a wide variety of research questions pertaining to PD; however, the number of studies failing to pass the MQC is alarming. Therefore, we provide recommendations to enhance the interpretability, generalizability, and clinical utility of future AI applications using neuroimaging in PD. },
keywords = {Artificial Intelligence, DaT imaging, Guidelines, Parkinson, Structural MRI},
pubstate = {published},
tppubtype = {article}
}